 I wrote previously about the hidden bioavailability analysis of GSK's new formulation of Eltroxin (thyroxine). These concerns followed multiple complaints from patients about side effects on the new formulation. Medsafe (the New Zealand drug regulator) had issued an alert, stating that:
I wrote previously about the hidden bioavailability analysis of GSK's new formulation of Eltroxin (thyroxine). These concerns followed multiple complaints from patients about side effects on the new formulation. Medsafe (the New Zealand drug regulator) had issued an alert, stating that:"In response to these reports, Medsafe has reassessed the change in Eltroxin formulation and can confirm that the new formulation satisfies all quality, safety, and bioequivalence criteria. In addition, all excipients and excipient quantities present in the new formulation are commonly used in medicines."GSK stated that
"extensive testing and retesting by GSK has shown that the tablets should be safe and effective when used as prescribed"However in response to my communications Medsafe refused to discuss what GSK's supposedly "extensive testing" was, the study design or the actual results - citing that the science "is commercial in confidence". Nor it seems were any of the data published in the scientific literature.
Now we have some information about these so called "extensive" tests, courtesy, not of usual science, but through response to a New Zealand parliamentary written question. Still no data, but it now seems that:
- Only 36 "test subjects" were studied.
- Studies lasted only 48 hours (perhaps long enough to determine bioavailability using measurements of T3 and T4 in blood - but in the absence of any details of study design or the actual results one cannot tell).
- It seems that "Almost 25% of the subjects experienced an adverse event when taking the new formulation of Eltroxin, compared to just 8% taking the standard formulation".
Member of Parliament Jackie Blue says "the authorities need to explain why this information did not ring alarm bells for them".
My questions would be more fundamental, regardless of the data. Why are we in this position in the first place, and what is the role of a scientific regulator?
See also the excellent Pharmalot on some aspects of this story
Earlier|Later|Main Page
 Recent problems with Eltroxin in New Zealand raise memories of a landmark scandal involving the researcher Betty Dong. Eltroxin is the brand name for levothyroxine (also known as thyroxine) as produced by GlaxoSmithKline.
Recent problems with Eltroxin in New Zealand raise memories of a landmark scandal involving the researcher Betty Dong. Eltroxin is the brand name for levothyroxine (also known as thyroxine) as produced by GlaxoSmithKline. The
The 
 I updated the
I updated the 
 I have taken a break over the past months while doing some more formal writing and (partially) recovering from illness. I ended up missing a whole lot of deadlines. The picture of
I have taken a break over the past months while doing some more formal writing and (partially) recovering from illness. I ended up missing a whole lot of deadlines. The picture of  Researchers have no 'right' to study terrorist materials, By Melanie Newman
Researchers have no 'right' to study terrorist materials, By Melanie Newman



 It's all very well blaming pharmaceutical companies for the decrepit state of integrity in medicine.
It's all very well blaming pharmaceutical companies for the decrepit state of integrity in medicine.

 Biomedical researchers at the University of Toronto are starting to sign a new
Biomedical researchers at the University of Toronto are starting to sign a new  f) Perhaps all of these codes serve as pretext for virtuous mumbling by groups whose very success is based on ethical failure. Morality they say is sometimes taught by the immoral. It is no surprise that Dr David Goldbloom at the University of Toronto (yes the one who fired Professor David Healy) lectures on ethical
f) Perhaps all of these codes serve as pretext for virtuous mumbling by groups whose very success is based on ethical failure. Morality they say is sometimes taught by the immoral. It is no surprise that Dr David Goldbloom at the University of Toronto (yes the one who fired Professor David Healy) lectures on ethical  "A good day ain't got no rain. A bad day's when I lie in bed and think of things that might have been."
"A good day ain't got no rain. A bad day's when I lie in bed and think of things that might have been."  One thing will be obvious to anyone who has spent time looking at scientific misconduct and academic bullying. Publicly known instances tend to aggregate within particular institutions.
One thing will be obvious to anyone who has spent time looking at scientific misconduct and academic bullying. Publicly known instances tend to aggregate within particular institutions.
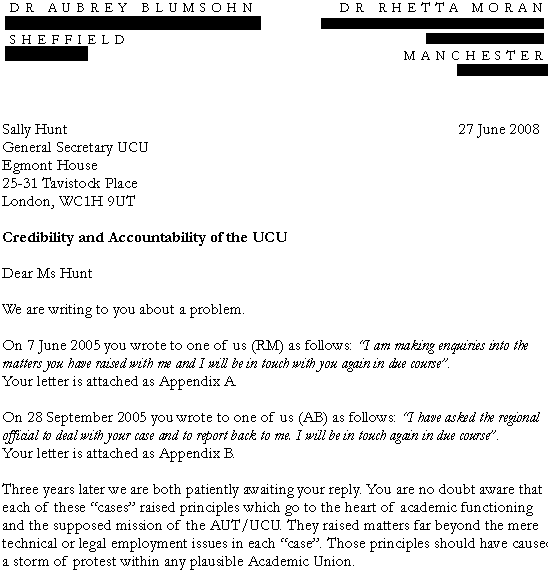

 My friend Rhetta Moran was fired from
My friend Rhetta Moran was fired from  Dr Rhetta Moran, 1 July 2008
Dr Rhetta Moran, 1 July 2008 I thought I would repeat the story of the thug and the policeman from the end of my previous post.
I thought I would repeat the story of the thug and the policeman from the end of my previous post. The Office for research integrity has just published a survey in Nature.
The Office for research integrity has just published a survey in Nature. Last week I received a tentative invitation (via the group Justice in Health) to "attend" an "event" at Westminster on 24 July 2008. The event "The Future of Health Professional Regulation" is hosted by the Council for Healthcare Regulatory Excellence (CHRE) and the Department of Health. It is supposedly about sorting out professional medical regulators in the interests of patients.
Last week I received a tentative invitation (via the group Justice in Health) to "attend" an "event" at Westminster on 24 July 2008. The event "The Future of Health Professional Regulation" is hosted by the Council for Healthcare Regulatory Excellence (CHRE) and the Department of Health. It is supposedly about sorting out professional medical regulators in the interests of patients.


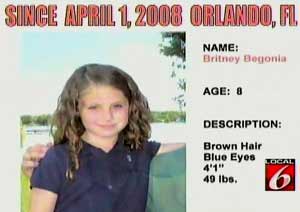 Local 6, a Florida TV station has been conducting
Local 6, a Florida TV station has been conducting